In this session, you'll explore the growing burden of benign prostatic hyperplasia (BPH) in ageing populations and discover why Prostatic Artery Embolisation (PAE) is emerging as a valuable, minimally invasive treatment option.Backed by global and South African clinical evidence, you'll learn how PAE addresses key challenges in resource-limited healthcare settings.
Overview
This narrative review provides an overview of benign prostatic hyperplasia (BPH), including its rising prevalence, clinical burden, and conventional management strategies. We then consider the evidence from two major international trials and a South African pilot study, demonstrating the efficacy and safety of PAE in both short- and long-term management of benign prostatic hyperplasia
Keywords: Benign Prostatic Hyperplasia, Prostatic Arterial Embolisation, Lower Urinary Tract Symptoms, Bladder Outlet Obstruction
The Escalating Impact of Benign Prostatic Hyperplasia
Benign prostatic hyperplasia (BPH) is a highly prevalent, chronic and progressive condition that affects older men, with increasing incidence after the fifth decade of life.¹ ²
Histologically, BPH is a multifocal process characterised by a non-malignant proliferation of both stromal and epithelial components within the prostate. This proliferation most commonly originates in the transitional zone of the gland, which surrounds the urethra. Over time, this leads to the formation of discrete nodules composed of hyperplastic tissue, often accompanied by chronic inflammation, glandular crowding, fibrosis, and increased smooth muscle tone.¹
These histological changes contribute to progressive urethral compression, resulting in bladder outlet obstruction (BOO). BOO, in turn, is often exacerbated by secondary changes in bladder function, particularly detrusor overactivity or underactivity due to chronic strain.
The clinical manifestations of this pathophysiology are referred to collectively as lower urinary tract symptoms (LUTS). These include urinary urgency, hesitancy, weak stream, increased frequency, nocturia, straining, and a sensation of incomplete emptying.¹
Importantly, BPH is not a uniform disease. It varies significantly in terms of gland size, symptom severity, and rate of progression, and it may occur concurrently with other causes of LUTS such as overactive bladder or prostate cancer. Understanding its anatomical origin, progressive nature, and clinical variability is essential for choosing appropriate management strategies.²
Epidemiology & Risk Factors
Histological studies estimate that benign prostatic hyperplasia (BPH) is present in up to 8% of men in their 40s, rising to 50% in their 60s, and affecting over 80% of men by their 80s. 2- 6 Longitudinal studies such as the Krimpen and Baltimore Aging Study have demonstrated that prostate volume—a key marker of BPH progression—increases annually by approximately 2–2.5% in older men. 2-5
This slow yet cumulative progression means that the vast majority of men will eventually experience some degree of LUTS related to BPH.
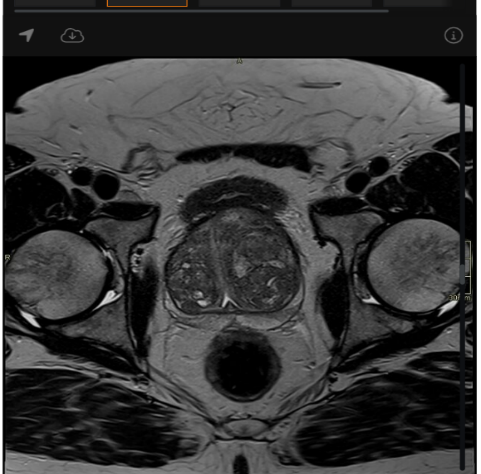
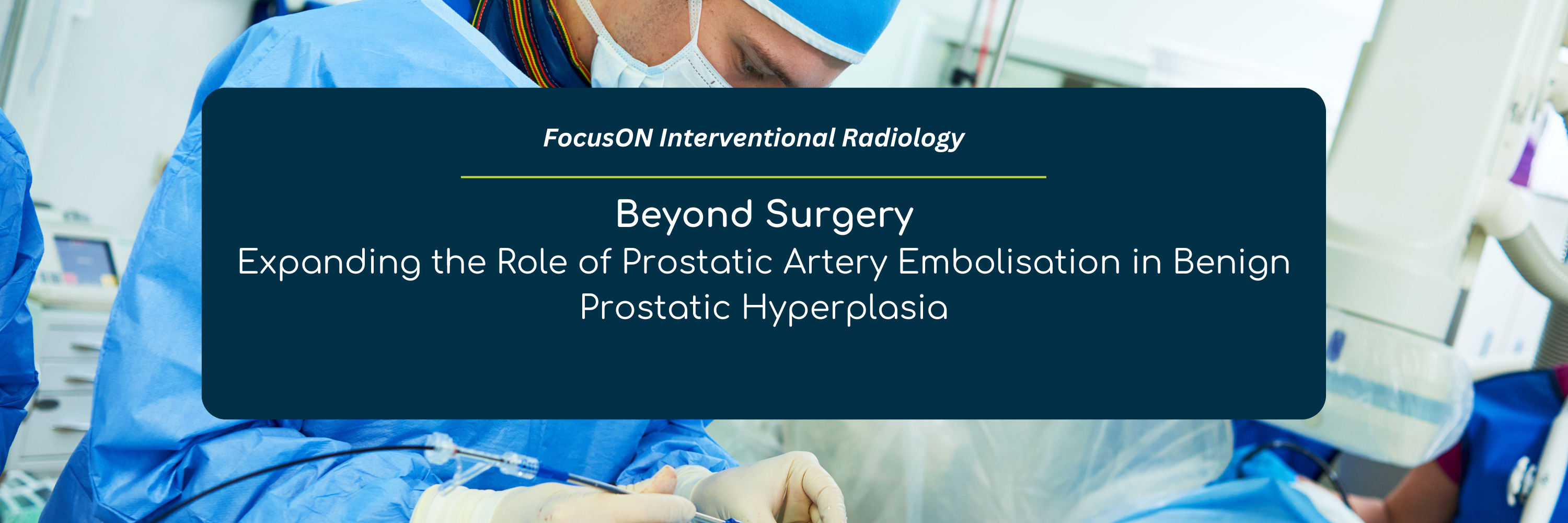
Figure 1: MRI of Benign Prostatic Hyperplasia (Click to open view)
Source: Bickle I, Benign prostatic hyperplasia. Case study, Radiopaedia.org (Accessed on 15 Jul 2025) https://radiopaedia.org/cases/206343/studies/161173
The use of certain medications—such as antidepressants, anticholinergics, and calcium channel blockers—has also been associated with increased risk.3 7 Lifestyle factors, particularly physical inactivity, poor diet, and excessive alcohol consumption, may accelerate symptom onset and progression.3 7 9Non-modifiable risk factors also play a significant role. These include genetic predisposition, family history, racial background, and socioeconomic or educational status.1 8 11
For example, BPH appears to be more common and potentially more severe among men of African descent, although global studies highlight regional variability in prevalence, diagnostic access, and health-seeking behaviour.10
Taken together, these findings underscore the complex and multifactorial nature of BPH—a disease shaped by biological ageing, comorbid conditions, lifestyle factors, and broader sociodemographic influences.
A Growing Public Health Concern In Low-and Middle-Income Countries
Benign prostatic hyperplasia is emerging as a significant public health challenge in low- and middle-income countries (LMICs), driven by population ageing and inadequate health infrastructure. In sub-Saharan Africa (SSA), where health systems are often overstretched, the clinical and economic burden of BPH is growing rapidly. 1 3 12 16
As far back as 2014, globally it was projected that LUTS and BOO would increase most steeply in SSA, with estimates indicating by as much as 20% by 2018, a trend primarily associated with demographic ageing in the region. 3 8 12
In South Africa, this trend is already visible: life expectancy has increased, with upto 70% of men over 80 reporting LUTS, and BPH established as the leading cause. Yet, national prevalence data remain limited, which hampers the planning of appropriate resources. 3 12 -16
Late presentation is common, driven by low public awareness and limited access to specialist care. Many patients first present with acute urinary retention (AUR) or renal impairment—indicating advanced disease and missed opportunities for early intervention. 3 12 -16
Data from the Global Burden of Disease Study show that between 2000 and 2019.2
- In South Africa, the rise was even steeper—74.3%
- Age-standardised prevalence increased modestly but significantly in both regions
The table below illustrates the growing prevalence of BPH over the last 20 years globally and in South and Sub-Saharan Africa
Table 1: GDB super-region and country-level prevelence of benign prostatic hyperplasia, and perecentage change between 2000 and 2019
Source: Awedew,Al Fentahun et al. The global, regional, and national burden of benign prostatic hyperplasia in 204 countries and territories from 2000 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Healthy Longevity, Volume 3, Issue 11, e754 - e776
Conventional Management Options and Limitations
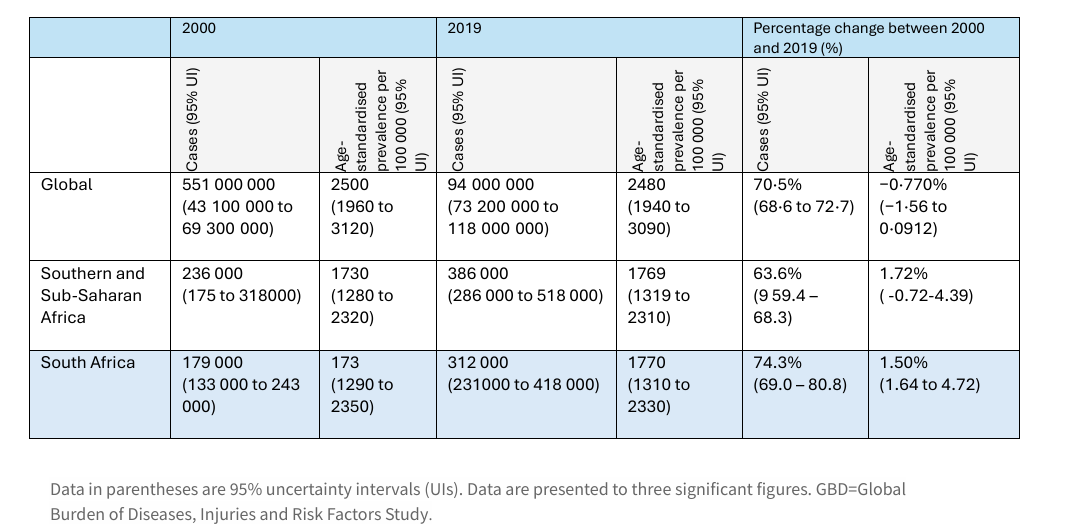
Figure 2: TURP defect (Click to open view)
Source: Morgan M, TURP defect. Case study, Radiopaedia.org (Accessed on 22 Jul 2025) https://doi.org/10.53347/rID-40682
The standard management of benign prostatic hyperplasia (BPH) includes lifestyle modifications, pharmacotherapy, and, when clinically indicated, surgical intervention.¹
Pharmacological treatment is usually the first-line approach. Alpha-blockers help relax the smooth muscle in the bladder neck and prostate to improve urinary flow, while 5-alpha-reductase inhibitors work by gradually reducing the prostate's volume.9 11 14-16
Although these agents can offer symptomatic relief, they are frequently associated with side effects, including dizziness, hypotension, and sexual dysfunction.
Adherence to long-term therapy is often poor, particularly in elderly patients with multiple comorbidities or those with limited access to regular follow-up. Furthermore, the long-term effectiveness of medical therapy can be inconsistent, especially in patients with progressive disease.
When conservative and medical therapies fail, or when urgent intervention is required—such as in cases of acute urinary retention (AUR), recurrent infections, or worsening bladder dysfunction—transurethral resection of the prostate (TURP) remains the gold standard.14
While TURP is highly effective in relieving symptoms and improving urinary flow, it is associated with a well-documented complication profile. Risks include perioperative bleeding, retrograde ejaculation, urinary incontinence, and cardiovascular strain from anaesthesia.
These risks are especially concerning in older, medically complex patients who may not tolerate surgery well. 2 9 12 Frail or elderly individuals with significant comorbidities—such as cardiovascular disease or diabetes—are often unsuitable for surgery due to elevated perioperative risk.
Neurological conditions like Parkinson’s disease, multiple sclerosis, or prior spinal cord injury complicate management further, due to associated bladder dysfunction and a heightened risk of postoperative incontinence. Patients on long-term anticoagulation therapy also present a challenge, as the bleeding risks of traditional surgical routes may outweigh the benefits—though alternatives like laser TURP can be considered in select cases.
Men with significantly enlarged prostates (>100 grams) are another difficult-to-manage group, often requiring specialised procedures such as HoLEP or open prostatectomy, which are not universally available. Additionally, patients with treatment-resistant LUTS—particularly those with overlapping bladder disorders or unrecognised prostate cancer—require comprehensive evaluation and individualised care plans.
According to the Global Burden of Diseases Study, the incidence of BPH in South Africa increased by 73% between 2000 to 2019 2
BPH care in LMICs is frequently hindered by financial and systemic barriers.
Although private healthcare facilities exist in countries like South Africa, the overwhelming majority of the population relies on the public health system for diagnosis and treatment.13 14
National health budgets in sub-Saharan Africa (SSA) allocate insufficient resources to conditions like BPH, which are not viewed as urgent or life-threatening. As a result, patients are frequently required to pay out-of-pocket for care—creating substantial financial barriers that delay intervention until complications, such as acute urinary retention or recurrent infections, arise. 3 7 15
South Africa’s public health system reflects these challenges. The volume of men requiring surgical management of BPH frequently exceeds available theatre capacity. Elective procedures, such as TURP, compete with higher-priority surgeries. According to a recent paper by Speis (2023), in some cases, BPH patients can wait up to three years for their surgery.
Such delays contribute to progressive symptom burden and a cascade of avoidable complications, including urinary infections, retention, and bladder dysfunction.7 11 12
Clinical and Economic Consequences
BPH’s impact extends far beyond the prostate. Men with moderate-to-severe LUTS are more likely to experience urinary tract infections, urolithiasis, acute urinary retention, and chronic kidney disease. The associated urgency, frequency, and nocturia impair sleep, reduce quality of life, and contribute to an increase in falls, depression, and sexual dysfunction.3 12 16 17
These burdens are shared by families and caregivers, amplifying the social and economic costs of the disease.
On a systemic level, BPH is becoming an increasingly costly condition. In 2019 alone, an estimated 11.26 million new cases were diagnosed globally. While LMIC-specific economic data are sparse, extrapolations from U.S. Medicare data suggest BPH-related medical service costs exceed USD 73.8 billion annually.² ³
For countries like South Africa, where surgical capacity is limited and health budgets are under immense pressure, this is unsustainable. As the older male population grows and more men seek treatment for symptomatic BPH, the burden on outpatient services, chronic medication supply, and surgical infrastructure will only increase.
The Need for Alternatives
The current model of BPH care is no longer sufficient to meet rising demand. Delayed interventions, high complication rates, and increasing costs point to the urgent need for accessible, minimally invasive therapies that can reduce symptom burden and system pressure. In resource-constrained settings, such alternatives are not just preferable—they are increasingly essential.
Back to top
Prostatic Artery Embolisation ( PAE): Minimally Invasive Therapeutic Option
Among these, Prostatic Artery Embolisation (PAE) has attracted growing clinical interest as an image-guided, organ-sparing procedure that offers symptom relief while avoiding many of the risks and extended recovery associated with traditional surgery.
PAE was originally developed for haemorrhage control, with its first reported use in the early 2000s. DeMeritt et al. described symptom improvement in a 76-year-old patient with intractable haematuria following embolisation of the prostatic arteries.18
Since then, the technique has undergone significant refinement. Where early approaches involved non-selective internal iliac embolisation, today’s procedures employ microcatheters to achieve precise, targeted occlusion of the prostatic arterial branches—a transformation that has both improved efficacy and minimised the risk of non-targeted embolisation. 9 16 20
Current Clinical Role and Technical Overview
Today, PAE is increasingly viewed as a first-line option for men with moderate-to-severe LUTS due to BPH, particularly those who are poor surgical candidates, those who wish to avoid invasive interventions or to prioritise preservation of erectile and ejaculatory function. 9,16,19
According to the Society of Interventional Radiology (SIR), PAE provides clinical outcomes that are comparable to surgical interventions, but with the additional benefits of shorter hospital stays, fewer transfusions, and low rates of sexual side effects.14
The procedure is typically performed via either a femoral or radial artery approach, utilising microcatheter techniques to selectively catheterise the prostatic arteries. Under fluoroscopic guidance, small, spherical polyvinyl alcohol (PVA) particles are then delivered to these vessels. This targeted embolisation induces ischaemic necrosis of the hyperplastic prostate tissue, leading to gradual volume reduction and symptomatic relief.14,16
Importantly, PAE is usually performed under local anaesthesia or conscious sedation, avoiding the risks associated with general anaesthesia. It also typically allows for short hospital stays – in some cases same-day discharges - making it a less invasive alternative to traditional surgical interventions. 9 14
Technique Optimisation
A key area of ongoing optimisation in PAE is the selection of embolic particle size, which can significantly influence both clinical efficacy and safety outcomes. Research by Bilhim et al. has demonstrated a meaningful trade-off in this regard.19
Larger particles (>200 µm) are associated with improved subjective symptom relief, such as International Prostate Symptom Score (IPSS) and peak urinary flow (Qmax), whereas smaller particles (<200 µm) appear to offer greater reductions in prostate-specific antigen (PSA) and overall prostate volume due to deeper arterial penetration.14,18
While initial concerns were raised about the potential for increased non-target embolisation with smaller particles, improvements in catheter design and procedural technique have largely mitigated these risks. Contemporary evidence now suggests that safety profiles are comparable across particle sizes when best practices are followed.14
This ability to tailor particle selection to the patient's anatomical and clinical profile may further enhance the safety and success of the procedure.
PAE provides clinical outcomes that are comparable to surgical interventions, but with the additional benefits of shorter hospital stays, fewer transfusions, and low rates of sexual side effects.14
A Viable Option for LMICs
As global evidence continues to accumulate, PAE is increasingly being viewed not just as a fallback for high-risk surgical patients, but as a front-line treatment for appropriately selected individuals.
As more interventional radiologists gain experience with prostate artery embolisation (PAE), its clinical utility is likely to expand—particularly in settings where surgical capacity is limited or patients face significant barriers to accessing operative care.
In resource-constrained environments such as South Africa’s public healthcare sector, PAE represents a compelling alternative: a minimally invasive, outpatient-based procedure that can help alleviate surgical backlogs while delivering meaningful symptom relief to men with BPH.12
While early outcomes are encouraging, the broader adoption of PAE depends on the accumulation of robust, long-term data to firmly establish its role within global BPH management algorithms. As comparative trials emerge and long-term outcomes become available, PAE has the potential to reshape the therapeutic landscape, offering a well-tolerated, effective solution that prioritises quality of life, functional outcomes, and patient-centred care.12 13
In Part Two of this paper, we will examine three key clinical trials—two international and one local—that provide valuable insight into the long-term efficacy of PAE and its impact on healthcare delivery within the South African context.
For more information on how Prostatic Artery Embolisation is transforming the treatment landscape for BPH, join Dr Dale Creamer and Dr Gareth Bydawell as they explore the clinical applications and emerging evidence behind this innovative therapy.
Back to top
Expanding the Evidence Base for Prostatic Artery Embolisation with Short-and Long-Term Data
To further evaluate the role of PAE, we considered three recent investigations that contribute valuable insights:
- A large, real-world, multicentre international study with 24-month follow-up; 20
- A high-volume, single-centre cohort tracked over nine years;21
- And a local South African case series conducted at Steve Biko Academic Hospital.13
They help illuminate the potential of PAE not only as a surgical alternative but as a scalable, sustainable solution to one of the most common urological challenges in ageing male populations worldwide.
Conducted across 14 centres in France, Italy, the United Kingdom, and the United States, it included 478 men aged 18 and older with symptomatic BPH, who presented either with LUTS or acute urinary retention (AUR). While the majority of the available PAE data has come from tightly controlled, single-centre settings, this registry was designed to reflect diverse clinical environments, patient demographics, and practice styles, thereby enhancing its applicability to routine care.
Participants underwent PAE using standardised techniques using microspheres delivered via femoral or radial access, typically under local anaesthesia.
Technical success, defined as the embolisation of at least one prostatic artery, was achieved in the vast majority of patients—91.6% in the LUTS cohort and 80.8% in the AUR cohort.
The results at 24 months demonstrated sustained, clinically meaningful improvements:
Quality of life (QoL) scores improved in tandem, and peak urinary flow (Qmax) increased by 5.3 mL/s (p < 0.001). Erectile function, as assessed by the SHIM questionnaire, remained stable—a key advantage when compared to TURP and other surgical modalities known for higher rates of sexual side effects.
Safety outcomes were reassuring:
Only 2.1% experienced serious AEs. Importantly, the re-embolisation rate was low (3.3%), and just 6.7% of patients required surgical or minimally invasive interventions within two years of their initial PAE.
By the study’s conclusion, clinical success—defined as an IPSS ≤15 or ≥25% reduction from baseline—was achieved in 79.3% of LUTS patients. These results align well with those of previous controlled studies and reinforce the growing endorsement of PAE by professional bodies, including the Society of Interventional Radiology and the American Urological Association.
The consistency of symptom improvement, low rate of reintervention, and excellent safety profile all support the broader adoption of PAE in real-world settings.
Disclaimer: This article is summarised here under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) Licence. This summary is for educational use only and does not alter or replace the original work. Readers are encouraged to consult the original publication for full details.
Extending the Horizon: A 9-Year Retrospective Review from a High-Volume Study
To address the pressing need for long-term data, a recent retrospective study published in March 2025 in the Journal of Vascular and Interventional Radiology by Bhatia, Shivank et al., conducted at the University of Miami, analysed the outcomes from 1,075 men who underwent PAE between January 2014 and July 2023.
As one of the longest-running and largest single-centre series to date, this study offers crucial evidence regarding the durability and safety of PAE over extended follow-up periods. Eligible participants included men with moderate-to-severe LUTS or AUR, often with prostate volumes exceeding 80 mL—a group historically managed surgically.
Notably, 130 patients had previously undergone procedures related to BPH, underscoring the heterogeneity and clinical complexity of the cohort. Men with advanced prostate cancer or significant renal dysfunction were excluded.
The majority of the procedures were completed via radial access. Cone-beam CT and fluoroscopic guidance were used to avoid non-target embolisation.
Protective coil embolisation was used in nearly 15% of patients to shield adjacent organs from unintended ischemia.
Follow-up extended to 60 months, with interim assessments at regular intervals.
Technical success was achieved in over 96% of cases.
QoL scores also improved dramatically and remained stable over time. This long-lasting benefit challenges earlier assumptions that PAE’s efficacy may wane over time and instead suggests that in carefully selected patients, the impact is not only comparable to but may rival the longevity of surgical outcomes.
The AUR subgroup further exemplified PAE’s utility.
PSA levels—often used as a surrogate measurement —declined by more than 50%, and prostate volumes shrank by over 30%.
Although some regrowth was noted beyond the 36-month point, the degree of improvement remained clinically significant.
Medication use also declined substantially.
Adverse events were rare and generally mild.
Serious adverse events occurred in fewer than 1% of patients and included three cases of transient ischaemic attacks, two of urosepsis and two patients with tissue slough requiring surgical intervention. All patients recovered fully.
Importantly, erectile function was preserved across the study population. IIEF-5 scores remained stable or even improved slightly, and no cases of new-onset erectile dysfunction were attributed to PAE. The preservation of sexual function is an increasingly important criterion for men seeking BPH treatment, and PAE is favoured compared to TURP, which carries a higher risk of sexual side effects.
By the fifth year, 16% of patients had undergone some form of reintervention.
Indeed, subgroup analysis revealed that men with prostate volumes >80 g fared just as well—if not better—than those with smaller glands, likely due to the deeper embolic penetration achievable in larger vascular territories.
Disclaimer: This article is summarised here under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Licence (CC BY-NC-ND 4.0). This summary is for educational use only and does not alter or replace the original work. Readers are encouraged to consult the original publication for full details
The South African Context: Local Evidence from a Public Sector Pilot Study
Fischer, H., Suleman, F., & Ahmad, S. (2019). Outcomes of prostate artery embolisation for benign prostatic hyperplasia in 10 cases at Steve Biko Academic Hospital. South African Journal of Radiology, 23(1), 6 pages. https://doi.org/10.4102/sajr.v23i1.1349
To obtain a local perspective, we therefore considered the 2019 retrospective review by Fisher et al., conducted at Steve Biko Academic Hospital (SBAH), which examined the outcomes of the first 10 PAE cases performed at the establishment.
The analysis assessed the safety, technical feasibility, and short-term efficacy of prostate artery embolisation (PAE) in men with lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH).
The cohort included 10 patients who underwent PAE between May and September 2016, all of whom were either refractory to medical therapy, deemed unfit for surgical intervention under general anaesthesia, or awaiting delayed surgical management due to theatre constraints within the South African public sector.
PAE was technically successful in all 10 patients (100%), with bilateral embolisation achieved in 9 (90%).
Embolisation was performed via femoral or radial artery access with super-selective catheterisation of the prostatic arteries using microcatheters. Embolic agents consisted of non-absorbable polyvinyl alcohol (PVA) particles. Non-target embolisation was minimised via coil protection of collateral branches to adjacent pelvic organs.
All patients were discharged within 24 hours after the procedure.
Outcomes were assessed at 3 months using standardised measures, including the International Prostate Symptom Score (IPSS), the American Urological Association (AUA) Quality of Life (QoL) scale, and prostate volume on magnetic resonance imaging (MRI).
Key findings included:
- IPSS: Mean improvement of 15.7 points, representing a 62% reduction in symptom burden (p < 0.0039).
- QoL: Mean improvement of 4.1 points on the AUA scale (72% reduction; p < 0.0039).
- Prostate Volume: Mean volumetric reduction of 29%, ranging from 4% to 77% (p < 0.0039), as assessed on MRI. One patient with a pacemaker was excluded from MRI-based volume analysis but demonstrated volume reduction on ultrasound.
These initial results suggest that PAE is both a technically viable and clinically effective intervention for selected patients with symptomatic BPH in a resource-constrained public healthcare setting.
The procedure offers meaningful symptom relief, reduction in prostate volume, and improved quality of life with a favourable safety profile, particularly in patients for whom traditional surgical options are contraindicated or inaccessible due to comorbidities or systemic capacity limitations
Although this is a small case series, the results align with international findings and suggest that PAE may offer a crucial therapeutic alternative in contexts where access to surgery is delayed or unavailable.
Disclaimer: This article is summarised here under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) Licence. This summary is for educational use only and does not alter or replace the original work. Readers are encouraged to consult the original publication for full details.
.Back to top
The Road Ahead - Building a Cumulative Case for PAE in BPH Management
Taken together, these three studies highlight the growing evidence base supporting PAE as a viable treatment for symptomatic BPH.
The short- and long-term clinical outcomes demonstrate consistent improvements in symptom burden, urinary function, and quality of life, with minimal risk to sexual health and low rates of reintervention.
In addition, the two international studies provide complementary perspectives: the study by Sapoval et al. underscores PAE’s safety, efficacy, and patient satisfaction in real-world, international contexts, whilst Bhatia et al. validate its long-term durability in a large, diverse cohort.
Both studies reaffirm that PAE is not merely a “bridge” treatment or fallback for high-risk surgical candidates, but rather a credible, evidence-based option in its own right. Its favourable side effect profile, minimal recovery time, and organ-sparing nature make it particularly attractive to men concerned about preserving sexual health and autonomy.
Additionally, the low rates of reintervention, steady improvement in both subjective and objective parameters, and significant decline in medication dependence argue for its inclusion earlier in the treatment pathway, not just as a last resort.
Critically, these findings also underscore the need to move beyond the traditional dichotomy between medical and surgical treatments for BPH. PAE occupies a middle ground: minimally invasive yet effective and durable.
As interventional radiology capacity expands and multidisciplinary collaboration deepens, PAE is poised to take on an increasingly central role in the management of BPH, both globally and locally.
In particular, as more interventional radiologists gain experience with this technique, its utility is likely to expand. In resource-constrained environments such as South Africa’s public sector, PAE represents a particularly promising option. It offers a minimally invasive, outpatient-based solution that can alleviate pressure on surgical theatres while delivering meaningful symptom relief to patients caught in extended care backlogs.
In conclusion, the evolving body of evidence suggests that Prostatic Artery Embolisation is not only here to stay but is rapidly establishing itself as a cornerstone of modern BPH management.
As more robust, comparative trials emerge and long-term data accumulate, PAE has the potential to fundamentally reshape the therapeutic landscape, offering men a well-tolerated, effective alternative that prioritises quality of life, functional outcomes, and patient choice.
Back to top
References
1.Ng M, Leslie SW, Baradhi KM. Benign Prostatic Hyperplasia. [Updated 2024 Oct 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558920/
2.Awedew, Atalel Fentahun et al. The global, regional, and national burden of benign prostatic hyperplasia in 204 countries and territories from 2000 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Healthy Longevity, Volume 3, Issue 11, e754 - e776 https://www.thelancet.com/journals/lanhl/article/PIIS2666-7568(22)00213-6/fulltext#tbl1
3.Cassell, A., Sine, B., Jalloh, M., & Gravas, S. (2024). Burden of Benign Prostatic Hyperplasia (BPH) in Low- and Middle-Income Countries in Sub-Saharan Africa (SSA). Société Internationale d’Urologie Journal, 5(5), 320-329. https://doi.org/10.3390/siuj5050051
4.Bosch, J. L., Tilling, K., Bohnen, A. M., Donovan, J. L., & Krimpen Study (2006). Establishing normal reference ranges for PSA change with age in a population-based study: The Krimpen study. The Prostate, 66(4), 335–343. https://doi.org/10.1002/pros.20293
5.Loeb, S., Kettermann, A., Carter, H. B., et al. (2009). Prostate volume changes over time: results from the Baltimore Longitudinal Study of Aging. The Journal of urology, 182(4), 1458–1462. https://doi.org/10.1016/j.juro.2009.06.047
6. Nickel J. C. (2003). Benign prostatic hyperplasia: does prostate size matter?. Reviews in urology, 5 Suppl 4(Suppl 4), S12–S17.
7.Ugare, U. G., Bassey, I. A., Udosen, E. J., Essiet, A., & Bassey, O. O. (2014). Management of lower urinary retention in a limited resource setting. Ethiopian journal of health sciences, 24(4), 329–336. https://doi.org/10.4314/ejhs.v24i4.8
8.Launer, B.M.; McVary, K.T.; Ricke, W.A.; Lloyd, G.L. The rising worldwide impact of benign prostatic hyperplasia. BJU Int. 2021, 127, 722–728. https://bjui-journals.onlinelibrary.wiley.com/doi/10.1111/bju.15286
9. Sapoval, M. Thiounn, N., Descazeud,A. et al.Prostatic artery embolisation versus medical treatment in patients with benign prostatic hyperplasia (PARTEM): a randomised, multicentre, open-label, phase 3, superiority trial The Lancet Regional Health – Europe, Volume 31, 100672 https://linkinghub.elsevier.com/retrieve/pii/S2666-7762(23)00091-1
10. Yeboah, E. D., & Hsing, A. W. (2016). BENIGN PROSTATIC HYPERPLASIA AND PROSTATE CANCER IN AFRICANS AND AFRICANS IN THE DIASPORA. Journal of the West African College of Surgeons, 6(4), x–xviii.https://pmc.ncbi.nlm.nih.gov/articles/PMC5667724/
11.Sandhu, J. S., Bixler, B. R., Dahm, P., et al.(2024). Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia (BPH): AUA Guideline Amendment 2023. The Journal of urology, 211(1), 11–19. https://doi.org/10.1097/JU.0000000000003698
12.Spies,P.V. The dawn of minimal invasive surgical therapies for benign prostate hyperplasia in South Africa: water vapour energy ablation with Rezum | African Urology Published Online:1 Jan 2023 https://doi.org/10.36303/AUJ.0032 https://journals.co.za/doi/full/10.36303/AUJ.0032
13.Fischer, H., Suleman, F., & Ahmad, S. (2019). Outcomes of prostate artery embolisation for benign prostatic hyperplasia in 10 cases at Steve Biko Academic Hospital. South African Journal of Radiology, 23(1), 6 pages. doi:https://doi.org/10.4102/sajr.v23i1.1349
14.Xhepa, G., Sciacqua, L. V., Vanzulli, A., Canì, A. E., et al. (2024). Prostate Artery Embolization (PAE) with Small Beads for the Treatment of Benign Prostatic Hyperplasia (BPH). Journal of personalized medicine, 14(6), 613. https://doi.org/10.3390/jpm14060613
15.Ahmed, H.U. et al. Cost Comparison of Surgical Interventions to TREAT Lower Urinary TRACT Symptoms (LUTS) Secondary to Benign Prostatic Hyperplasia (BPH) in the UK, Sweden, and South Africa Value in Health, Volume 23, S580 https://www.valueinhealthjournal.com/article/S1098-3015(20)33316-7/fulltext
16.Yu, H., Isaacson, A. J., & Burke, C. T. (2016). Review of Current Literature for Prostatic Artery Embolization. Seminars in interventional radiology, 33(3), 231–235. https://doi.org/10.1055/s-0036-1586141
17.Husted, M., Gray, D., Golding, S. E., & Hindley, R. (2022). Reaching a Tipping Point: A Qualitative Exploration of Quality of Life and Treatment Decision-Making in People Living With Benign Prostatic Hyperplasia. Qualitative health research, 32(13), 1979–1992. https://doi.org/10.1177/10497323221129262
18.DeMeritt J S, Elmasri F F, Esposito M P, Rosenberg G S. Relief of benign prostatic hyperplasia-related bladder outlet obstruction after transarterial polyvinyl alcohol prostate embolization. J Vasc Interv Radiol. 2000;11(6):767–770. doi: 10.1016/s1051-0443(07)61638-8. https://linkinghub.elsevier.com/retrieve/pii/S1051044307616388
19. Bilhim, T., Costa, N. V., Torres, D., Pinheiro, L. C., & Spaepen, E. (2022). Long-Term Outcome of Prostatic Artery Embolization for Patients with Benign Prostatic Hyperplasia: Single-Centre Retrospective Study in 1072 Patients Over a 10-Year Period. Cardiovascular and interventional radiology, 45(9), 1324–1336. https://doi.org/10.1007/s00270-022-03199-8
20.Sapoval, M. R., Bhatia, S., Déan, C. et al, & PROstate Study Investigators (2024). Two-Year Outcomes of Prostatic Artery Embolization for Symptomatic Benign Prostatic Hyperplasia: An International, Multicenter, Prospective Study. Cardiovascular and interventional radiology, 47(11), 1515–1524. https://doi.org/10.1007/s00270-024-03802-0
21. Bhatia, S., Bhatia, A., Richardson, A. J., et al. (2025). Prostatic Artery Embolization: Mid- to Long-Term Outcomes in 1,075 Patients. Journal of vascular and interventional radiology : JVIR, 36(3), 456–466. https://doi.org/10.1016/j.jvir.2024.11.002
Back to top
Copyright
This article is made available under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (CC BY-NC 4.0). This permits non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Commercial use is not permitted without prior written permission from the author(s). For more information contact admin@meded.co.za
Publication Information
Published: 16 July 2025
Catalogue Number: MRN007
Category: Radiology
Sub-Category: Interventional Radiology, Men's Health
Fact-Checked: 15 July 2025
Corresponding Author: Ravenhill, L
Disclaimer
Every effort has been made to attribute quotes and content correctly. Where possible, all information has been independently verified. The Medical Education Network bears no responsibility for any inaccuracies which may occur from the use of third-party sources. If you have any queries regarding this article contact us
Fact-checking Policy
The Medical Education Network makes every effort to review and fact-check the articles used as source material in our summaries and original material. We have strict guidelines in relation to the publications we use as our source data, favouring peer-reviewed research wherever possible. Every effort is made to ensure that the information contained here accurately reflects the original material. Should you find inaccuracies or out-of-date content or have any additional issues with our articles, please make use of the Contact Us form to notify us.