Clinical Summary | Anaesthetics
The role of perioperative sedative anesthetics in preventing postoperative delirium: a systematic review and network-meta analysis
Time to read: 07:16 minutes
Time to listen: 11:33 minutes
Originally Published: 6 March 2024
Source: BMC Cardiovascular Disorders
Type of article: Clinical Research Summary
MedED Catalogue Reference: MCECS014
Category: Anaesthesia
Cross-reference: Neurology, Surgery
Keywords: anaesthesia, surgery, cardiology, delirium, cognitive decline
Key Take Aways
1. Various factors, including age, type of surgery, and duration of intubation influence postoperative delirium.
2. Dexmedetomidine is effective in preventing postoperative delirium in both cardiac and non-cardiac surgeries.
3. The preventive effect of dexmedetomidine is more pronounced with longer surgical and extubation times.
4. Close monitoring is required during dexmedetomidine administration due to its association with bradycardia
Top
Study Context | Objectives | Study Design | Findings | Discussion| Limitations | Conclusion | Original Research | Funding | References
Study Context
Postoperative delirium, also known as postoperative cognitive dysfunction (POCD), is a common complication after surgery, particularly in the elderly, with an incidence rate as high as 70%.1 It typically arises within 1 to 3 days post-surgery and can persist for 2 to 5 days, leading to prolonged hospitalisation, increased healthcare costs, and higher mortality rates. 2,3Back to top
Study Purpose
The stated purpose of this study is to " .. investigate whether there is an effective sedative that can prevent postoperative delirium while also examining the safety of using sedatives during the perioperative period.”
Back to top
Study Design
This study employed a net-meta-analysis to compare the incidence of postoperative delirium among the four anaesthetics agents namely: sevoflurane, propofol, dexmedetomidine, and midazolam.
Randomised control trials were selected based on the following specific criteria:
Back to top
Findings
Of the initial 4012 articles initially identified, 41 studies met the inclusion criteria, accounting for a total of 6679 patients:
- Twelve of the studies focused on cardiac surgery, 28 on non-cardiac surgery, and 1 on both cardiac and non-cardiac surgery.
- Six studies were conducted in the ICU, 33 studies were conducted in the OR, and two studies included both OR and ICU settings.
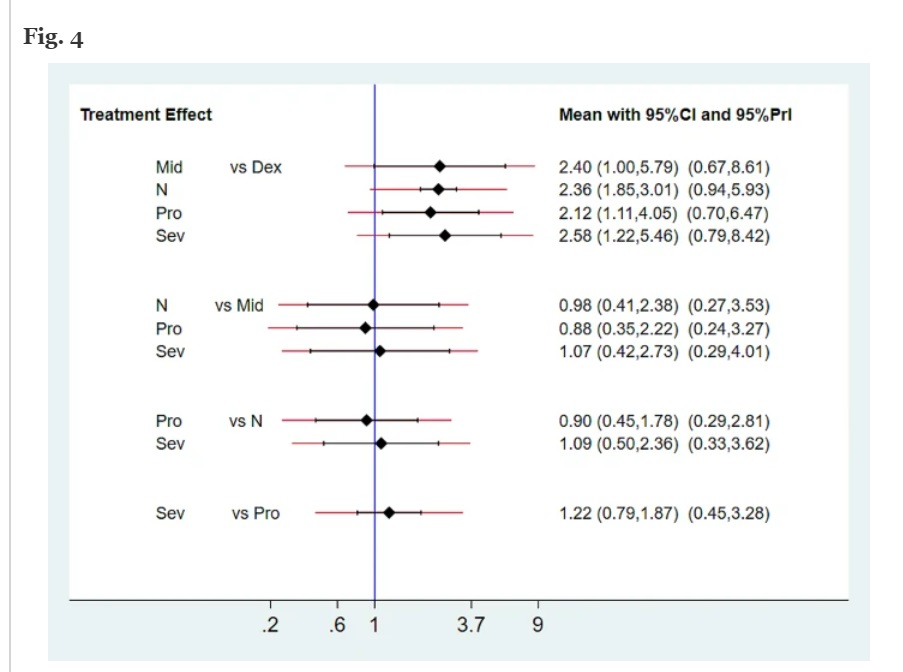
Click on the image to enlarge
Source: Huang, J. X.& Zhang, et al (2024). The role of perioperative sedative anesthetics in preventing postoperative delirium: a systematic review and network-meta analysis including 6679 patients. BMC cardiovascular disorders, 24(1), 147. https://doi.org/10.1186/s12872-024-03783-5
1. Dexmedetomidine administered within the first hour after surgery was more effective at preventing postoperative delirium compared to midazolam (OR 15.55; 95% CI 1.11-218.13) and normal saline (OR 3.48; 95% CI 1.75-6.94).
In sub-analysis:
2. For surgeries lasting more than three hours, dexmedetomidine showed a significantly better preventive effect on postoperative delirium than other anaesthetic regimens.
Results indicated that patients receiving midazolam (OR 3.34; 95% CI 2.04–5.48) and normal saline (OR 2.27; 95% CI 1.17–4.39) had a higher likelihood of developing postoperative delirium compared to those treated with dexmedetomidine.
4. Additional Secondary outcomes
Bradycardia was reported in 12 articles involving 1,831 participants, with a significantly lower incidence in the saline group compared to the dexmedetomidine group (OR 0.55; 95% CI 0.37 to 0.80). There were no significant differences in the incidence of bradycardia among other sedatives.
Additionally, of the 41 articles analysed, only 12 reported instances of hypotension, and the rates of hypotension for various drugs were not statistically significant.
Discussion
The researchers conclude that their analysis supports previous research and guidelines, which indicate that dexmedetomidine can effectively reduce the incidence of postoperative delirium.
Limitations
Back to top
Conclusion
Access the original research
Huang, J. X., Zhang, S. S., Wang, S. X., Xi, D. S., Luo, F. R., Liu, C. J., & Li, H. (2024). The role of perioperative sedative anesthetics in preventing postoperative delirium: a systematic review and network-meta analysis including 6679 patients. BMC cardiovascular disorders, 24(1), 147. https://doi.org/10.1186/s12872-024-03783-5
Back to top
Conflict of Interest, Funding and Support
Role of the Funder/Sponsor
The study's funder had no role in the design, data collection, data analysis, data interpretation, or writing of the report.
Conflict of Interest Disclosures
Funding/Support
The research was funded by the National Nature funding (No:82171265).
References
1. Saleh, A. J., Tang, G. X., Hadi, S. M., Yan, L., Chen, M. H., Duan, K. M., Tong, J., & Ouyang, W. (2015). Preoperative cognitive intervention reduces cognitive dysfunction in elderly patients after gastrointestinal surgery: a randomised controlled trial. Medical science monitor : international medical journal of experimental and clinical research, 21, 798–805. https://doi.org/10.12659/MSM.893359
2. Saczynski, J. S., Marcantonio, E. R., Quach, L., Fong, T. G., Gross, A., Inouye, S. K., & Jones, R. N. (2012). Cognitive trajectories after postoperative delirium. The New England journal of medicine, 367(1), 30–39. https://doi.org/10.1056/NEJMoa1112923
3. Rengel, K. F., Pandharipande, P. P., & Hughes, C. G. (2019). Special Considerations for the Aging Brain and Perioperative Neurocognitive Dysfunction. Anesthesiology clinics, 37(3), 521–536. https://doi.org/10.1016/j.anclin.2019.04.010
Disclaimer
This article is in no way presented as an original work. Every effort has been made to attribute quotes and content correctly. Where possible, all information has been independently verified. The Medical Education Network bears no responsibility for any inaccuracies which may occur from the use of third-party sources. If you have any queries regarding this article contact us
Fact-checking Policy
The Medical Education Network makes every effort to review and fact-check the articles used as source material in our summaries and original material. We have strict guidelines in relation to the publications we use as our source data, favouring peer-reviewed research wherever possible. Every effort is made to ensure that the information contained here accurately reflects the original material. Should you find inaccuracies or out-of-date content or have any additional issues with our articles, please make use of the Contact Us form to notify us.