Clinical examination alone cannot reliably exclude spinal injury and tends to overestimate injury level. The low negative predictive values mean that normal motor and sensory findings do not adequately rule out significant pathology. Imaging remains essential: CT for bony assessment and MRI for soft tissue, ligamentous, and spinal cord evaluation. Combined clinical and radiological assessment provides the most accurate foundation for management decisions, including surgical intervention (favoured within 24 hours for unstable fractures), conservative treatment, and coordinated multidisciplinary care.
In Brief | Radiology & Imaging, Emergency Medicine
Radiology & Emergency Medicine: Evaluating the Accuracy of Clinical Examination Against Imaging in Spinal Trauma. A South African Study
2 February 2026
Clinical motor and sensory examination moderately predicts spinal injury, but imaging (CT and MRI) remains essential to accurately identify injury level and detect subtle or soft-tissue injuries.
Quick Facts
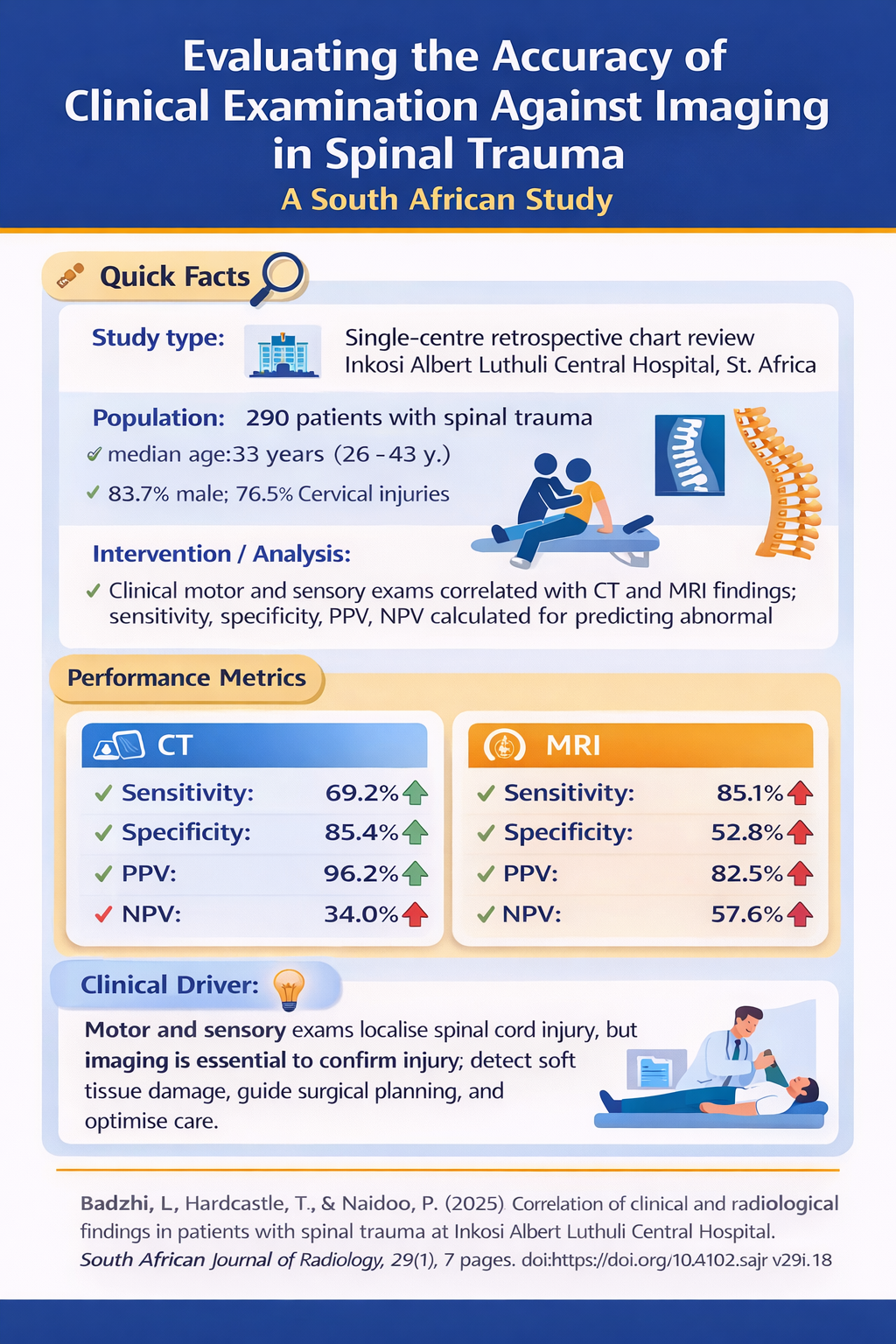
- Study type: Single-centre retrospective chart review (Inkosi Albert Luthuli Central Hospital, 6 years)
Population: 290 patients with spinal trauma (median age 33 years; 83.7% male; 76.5% cervical injuries)
Interventions / Analysis: Clinical motor and sensory examination correlated with CT and MRI findings; sensitivity, specificity, PPV, NPV calculated for predicting abnormal imaging
Key result: Clinical findings reasonably predict abnormal imaging but cannot reliably exclude injury; CT best for bony injuries, MRI best for soft tissue and spinal cord evaluation
Performance metrics:- CT: Sensitivity 69.2%, Specificity 85.4%, PPV 96.2%, NPV 34.0%
- MRI: Sensitivity 85.1%, Specificity 52.8%, PPV 82.5%, NPV 57.6%
- Clinical driver: Clinical examination helps localise spinal cord injury, but imaging is essential to confirm injury, detect subtle soft tissue damage, guide surgical planning, and optimise multidisciplinary management
Top
Study Context
Spinal trauma is increasingly common in South Africa, particularly among young males. In this study of 290 patients at Inkosi Albert Luthuli Central Hospital, 83.7% were male with a median age of 33 years.
Cervical spine injuries predominated (76.5%), with thoracic injuries accounting for 13.8% and lumbo-sacral or multilevel injuries comprising approximately 10%. Vehicle-related mechanisms (motor vehicle collisions and pedestrian vehicle crashes) caused 61.8% of injuries. Polytrauma was the norm rather than the exception: over 70% had concurrent brain injuries, 37.5% chest injuries, 28.6% abdominal injuries, and 37.2% limb injuries.
Spinal trauma assessment traditionally relies on comprehensive neurological examination using the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) and ASIA impairment scale.
However, the accuracy of clinical assessment versus radiological findings, and whether imaging is always necessary, remain important clinical questions—particularly in resource-constrained settings where advanced imaging may be limited.
Study Objective
To evaluate whether clinical motor and sensory findings correlate with imaging results, determine if imaging is always necessary, and compare the predictive accuracy of clinical versus radiological assessment in spinal trauma patients.
Study Methodology
This retrospective chart review analysed 290 patients with spinal injuries admitted over six years (2018–2024) who received CT and/or MRI. Motor and sensory examination findings were compared against radiological results.
Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated to assess the clinical examination's ability to predict abnormal imaging findings.
Study Findings
Clinical motor and sensory findings demonstrated high positive predictive value but concerning limitations in ruling out injury.
For CT imaging, clinical findings showed 69.2% sensitivity, 85.4% specificity, 96.2% PPV, but only 34.0% NPV. For MRI, sensitivity improved to 85.1%, with 52.8% specificity, 82.5% PPV, and 57.6% NPV.
Clinical findings correlated with abnormal CT results in 84.4% of cases and with MRI in 72.3%—suggesting reasonable agreement but revealing a critical gap: clinical examination frequently overestimated the injury level or position.
The low negative predictive values (34.0% for CT, 57.6% for MRI) indicate that negative clinical findings cannot reliably exclude spinal injury.
CT proved superior for detecting bony injuries, fractures, subluxations, and dislocations, while MRI was essential for identifying soft tissue pathology—including posterior and anterior ligamentous injuries, spinal cord oedema, haemorrhage, and disc ruptures.
Some patients presented with Spinal Cord Injury Without Radiographic Abnormality (SCIWORA), where neurological deficits existed despite normal CT findings, making MRI crucial for diagnosis.
Why This is Relevant for South African Practitioners
This study reinforces that while neurological examination using ISNCSCI/ASIA protocols helps localise spinal cord injury, it cannot replace imaging. Both CT and MRI add crucial diagnostic detail that clinical findings alone miss or mischaracterize, supporting their continued essential role in trauma protocols—even in resource-limited settings where their use must be strategically prioritised.
Original Study
Badzhi, L., Hardcastle, T., & Naidoo, P. (2025). Correlation of clinical and radiological findings in patients with spinal trauma at Inkosi Albert Luthuli Central Hospital. South African Journal of Radiology, 29(1), 7 pages. doi:https://doi.org/10.4102/sajr.v29i1.3248
The content in this summary is intended as an overview only and does not replace the original research. Members should review the original study before forming clinical opinions. The Medical Education Network cannot be held liable for inaccuracies or omissions.
Fact-checking Policy:
The Medical Education Network makes every effort to review and fact-check source material. Please use the contact us form to report issues.


