Retinal imaging during routine ROP screening may offer a non-invasive biomarker for early detection of BPD and PH. Integrating retinal oculomics with clinical data could allow earlier, individualized intervention, reduce reliance on invasive testing, and improve risk stratification in very preterm infants.
In Brief | Ophthalmology, Paediatrics, Cardiology, LLM
Ophthalmology: Can Retinal Images Predict Cardiopulmonary Disease in Preterm Infants?
28 January 2026
Keywords: Bronchopulmonary dysplasia Pulmonary Hyertension OculomicsNeonatal Medicine
Retinal images from routine ROP screening contain predictive signals for bronchopulmonary dysplasia (BPD) and pulmonary hypertension (PH) in preterm infants. Combining imaging features with demographic risk factors improves prediction compared with demographics alone, suggesting a potential non-invasive biomarker for earlier diagnosis and targeted care.
Quick Facts
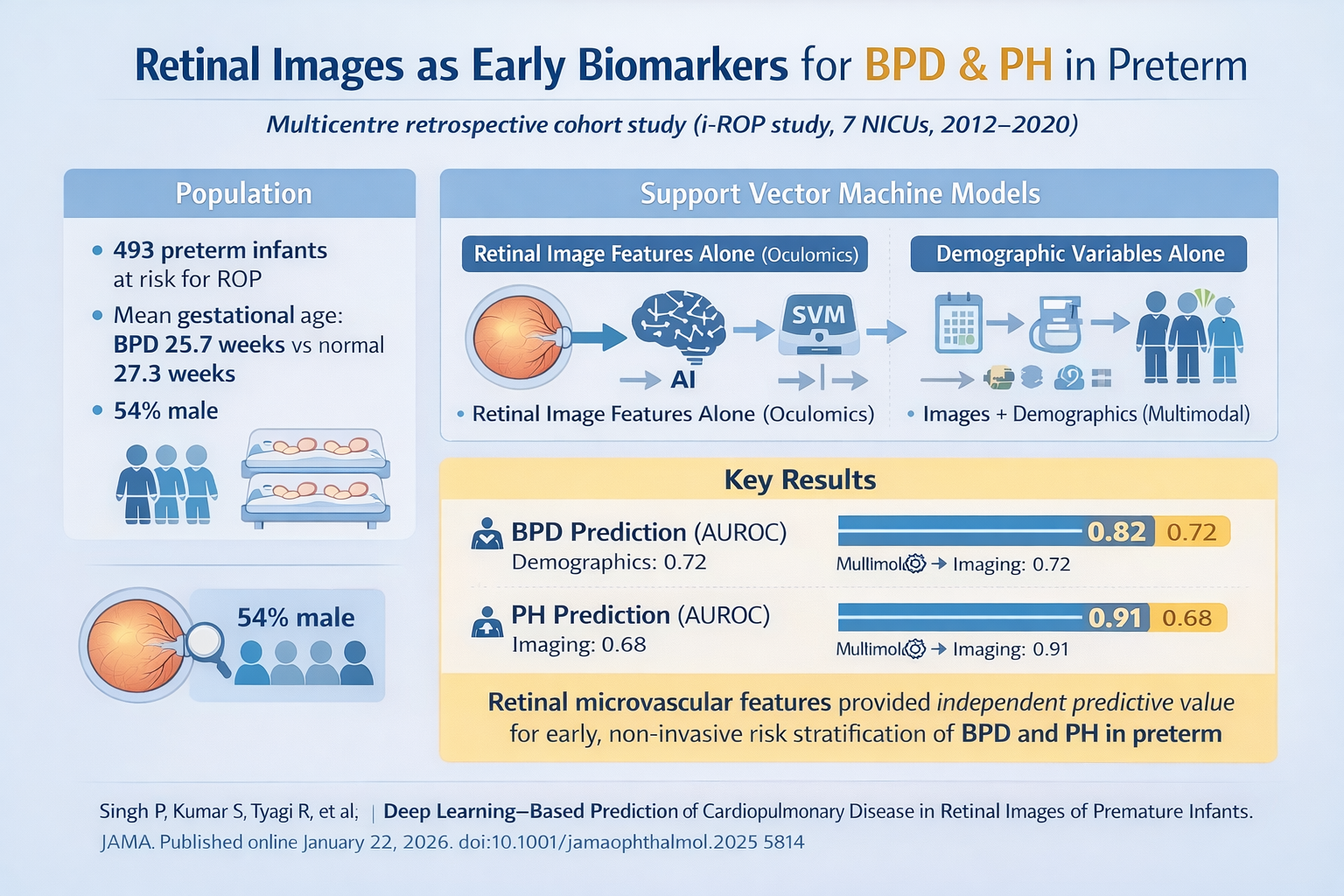
- Study type: Multicentre retrospective cohort study (i-ROP study, 7 NICUs)
- Population: 493 preterm infants at risk for ROP (mean gestational age: BPD 25.7 weeks vs normal 27.3 weeks; 54% male)
- Interventions / Analysis: Support vector machine models using (1) retinal image features alone, (2) demographic variables alone, (3) multimodal combination of images + demographics; secondary analysis excluded images with clinical ROP
- Key result: Multimodal models improved the prediction of BPD and PH compared with demographics alone
- Performance metrics (AUROC):
- BPD: Multimodal 0.82 vs demographics-only 0.72; imaging-only 0.72
- PH: Multimodal 0.91 vs demographics-only 0.68; imaging-only 0.91
- Clinical driver: Retinal microvascular features (vessel calibre, branching, and tortuosity) provide independent predictive value for systemic pulmonary and vascular disease, supporting early non-invasive risk stratification
Top
Study Summary
BPD affects ~1/3 of very preterm infants and contributes to prolonged ventilation, oxygen dependence, and long-term pulmonary and neurodevelopmental morbidity. PH, often coexisting with BPD, carries high mortality (up to 50% within 2 years in severe cases).
Traditional prediction relies on demographic and clinical factors (gestational age, birth weight, oxygen exposure) but is not reliably actionable. PH diagnosis typically requires echocardiography or invasive cardiac catheterisation.
Retinal imaging, already integrated for ROP screening, could serve as a non-invasive window into systemic microvascular health using deep learning (“oculomics”).
Study Objective
To evaluate whether ROP screening images contain features linked to BPD and PH, and whether a multimodal imaging-demographic model outperforms demographic risk factors alone.
Study Methodology
This multi-institutional study analysed retinal images from the i-ROP cohort (7 NICUs, 2012–2020). Only images ≤34 weeks’ PMA were included to precede BPD or PH diagnosis.
BPD diagnosis required continued oxygen dependency at 36 weeks PMA, while PH diagnosis relied on echocardiographic findings at 34 weeks.
A support vector machine model was trained using: (1) image features (via ResNet18), (2) demographic variables (gestational age, birth weight, sex, race/ethnicity), and (3) a multimodal combination.
Secondary analyses excluded images with ROP signs to reduce confounding. Performance was assessed using AUROC on held-out test sets.
Study Findings
493 infants were included (mean GA: BPD 25.7 weeks vs normal 27.3 weeks; 54% male).
The study tested three prediction approaches: (1) retinal imaging alone, (2) standard clinical factors alone (gestational age, birth weight, sex, race/ethnicity), and (3) a combined approach using both.
For BPD prediction:
- The combined model achieved good predictive accuracy (AUC 0.82)
- This outperformed either clinical factors alone or retinal imaging alone (both AUC 0.72, fair accuracy)
- Clinical significance: Combining retinal images with routine clinical data improves risk prediction by approximately 14%
- The combined model achieved excellent predictive accuracy (AUC 0.91)
- Retinal imaging alone was equally effective (AUC 0.91)
- Clinical factors alone showed only fair accuracy (AUC 0.68)
- Clinical significance: Retinal images were highly predictive of PH independent of traditional risk factors
Importantly, these results held even when images showing ROP changes were excluded, confirming that the retinal vascular patterns provide distinct predictive information beyond ROP status.
**AUROC interpretation guide: 0.5 = no better than chance; 0.7 = fair; 0.8 = good; 0.9 = excellent
Retinal imaging during routine ROP screening may offer a non-invasive biomarker for early detection of BPD and PH. Integrating retinal oculomics with clinical data could allow earlier, individualized intervention, reduce reliance on invasive testing, and improve risk stratification in very preterm infants.
Why is this relevant for South African Practitioners?
Extremely low-birthweight (ELBW; <1,000g) neonates in South Africa face high mortality and morbidity. In their 2021 study, Musiime et al. investigated all live-born ELBW neonates treated at Tygerberg Hospital between 1 January and 31 December 2016 - a total sample of 256 neonates -and reported that BPD affected 8.2% and ROP 31% of survivors at this tertiary centre.1
The high burden of respiratory and vascular complications, coupled with limited access to advanced diagnostic resources, underscores the need for non-invasive, predictive tools.
Oculomics-based risk stratification could identify infants at the highest risk for BPD or PH early, enabling closer monitoring, optimisation of respiratory support, and targeted referral for echocardiography, potentially improving survival and long-term outcomes in South African NICUs.
Original Study
References
The content in this summary is intended as an overview only and does not replace the original research. Members should review the original study before forming clinical opinions. The Medical Education Network cannot be held liable for inaccuracies or omissions.
Fact-checking Policy:
The Medical Education Network makes every effort to review and fact-check source material. Please use the contact us form to report issues.


