PTCy appears to mitigate the adverse impact of increasing unrelated donor age on post-transplant survival. In contrast to conventional CNI prophylaxis, older donor age did not significantly worsen outcomes when PTCy was used. This suggests that the longstanding emphasis on younger, unrelated donors may be less critical in the era of PTCy-based GVHD prophylaxis.
In Brief | Transplant Medicine, Oncology, Haematology
Transplant Medicine: Donor Age and Outcomes After Unrelated Donor Transplantation in the Post-Transplant Cyclophosphamide Era
19 January 2026
Posttransplant cyclophosphamide appears to mitigate the adverse impact of older unrelated donor age on survival, challenging the traditional priority for younger donors in allogeneic HCT.
Quick Facts
- Study type: Multicentre retrospective cohort study (CIBMTR registry)
- Population: 10 025 adults undergoing unrelated donor allogeneic HCT (mean age 56.5 years)
- Interventions: GVHD prophylaxis with calcineurin inhibitors (CNI) vs post-transplant cyclophosphamide (PTCy)
- Key result: Increasing donor age was associated with worse overall survival in CNI-based MUD and MMUD transplants, but not in PTCy-based transplants
- Hazard ratios:
- MUD-CNI: HR 1.004–1.009 per year increase in donor age
- MMUD-CNI: HR 1.022–1.034 per year
- PTCy cohorts: no significant association
- Clinical driver: The attenuation of donor age risk with PTCy was primarily driven by stable non-relapse mortality across donor ages
Top
Study Objective
To evaluate whether the impact of older unrelated donor (URD) age on overall survival varies between patients receiving post-transplant cyclophosphamide (PTCy)–based graft-versus-host disease (GVHD) prophylaxis versus conventional calcineurin inhibitor (CNI)–based prophylaxis.
Study Summary
Advanced age in unrelated donors has long been recognised as a risk factor for poorer survival after allogeneic haematopoietic cell transplantation (HCT). Traditionally, transplant protocols have prioritised younger donors when using conventional calcineurin inhibitor (CNI)–based GVHD prophylaxis.
In recent years, wider use of post-transplant cyclophosphamide (PTCy) has effectively reduced GVHD, raising the question of whether donor age still affects outcomes. Mehta et al. addressed this question in their study.
Study Design
This large, multicentre retrospective cohort study used data from the Centre for International Blood and Marrow Transplant Research (CIBMTR).
Adult patients with acute leukaemia or myelodysplastic syndrome who underwent unrelated donor allogeneic HCT between January 2017 and June 2021 were included.
Patients received either matched (8/8 HLA) or mismatched (7/8 HLA) unrelated donor grafts with GVHD prophylaxis consisting of either CNI-based regimens or PTCy-based regimens. Donor age was analysed as a continuous variable.
The primary outcome was overall survival (OS). Multiple analytic approaches were used, including standard and overlap-weighted inverse probability of treatment weighting (IPTW), LASSO-penalised Cox regression, and machine-learning–based XGBoost modelling.
The analysis included 10,025 patients (mean [SD] age, 56.5 [14.4] years), comprising 4379 women (43.7%) and 5646 men (56.3%).
- Matched unrelated donor with CNI prophylaxis (MUD-CNI): 7272 patients (72.5%)
- Matched unrelated donor with PTCy (MUD-PTCy): 1681 patients (16.8%)
- Mis-matched unrelated donor with PTCy (MMUD-PTCy): 613 patients (6.1%)
- Mis-matched unrelated donor with CNI (MMUD-CNI): 459 patients (4.6%)
Study Findings
Among patients receiving CNI-based GVHD prophylaxis, increasing donor age was consistently associated with worse overall survival.
In the matched unrelated donor with PTCy (MUD-CNI) cohort, each additional year of donor age was associated with a statistically significant increase in mortality risk (hazard ratio [HR], 1.004–1.009 per year) .
This association was more pronounced in the mis-matched unrelated donor (MMUD-CNI) cohort, where increasing donor age was associated with substantially worse survival outcomes (HR, 1.022–1.034 per year).
In contrast, no significant association between donor age and OS was observed in patients receiving PTCy-based GVHD prophylaxis. In the combined PTCy cohort, donor age was not associated with inferior survival (HR, 1.001–1.007 per year), indicating a clear attenuation of donor age–related risk.
These findings were consistent and robust across all statistical and machine-learning approaches employed, including IPTW, LASSO-penalised regression, and XGBoost analyses. Further analyses demonstrated that the attenuation of donor age effects in the PTCy cohort was primarily driven by non-relapse mortality, with no observed association between increasing donor age and non-relapse mortality among PTCy recipients.
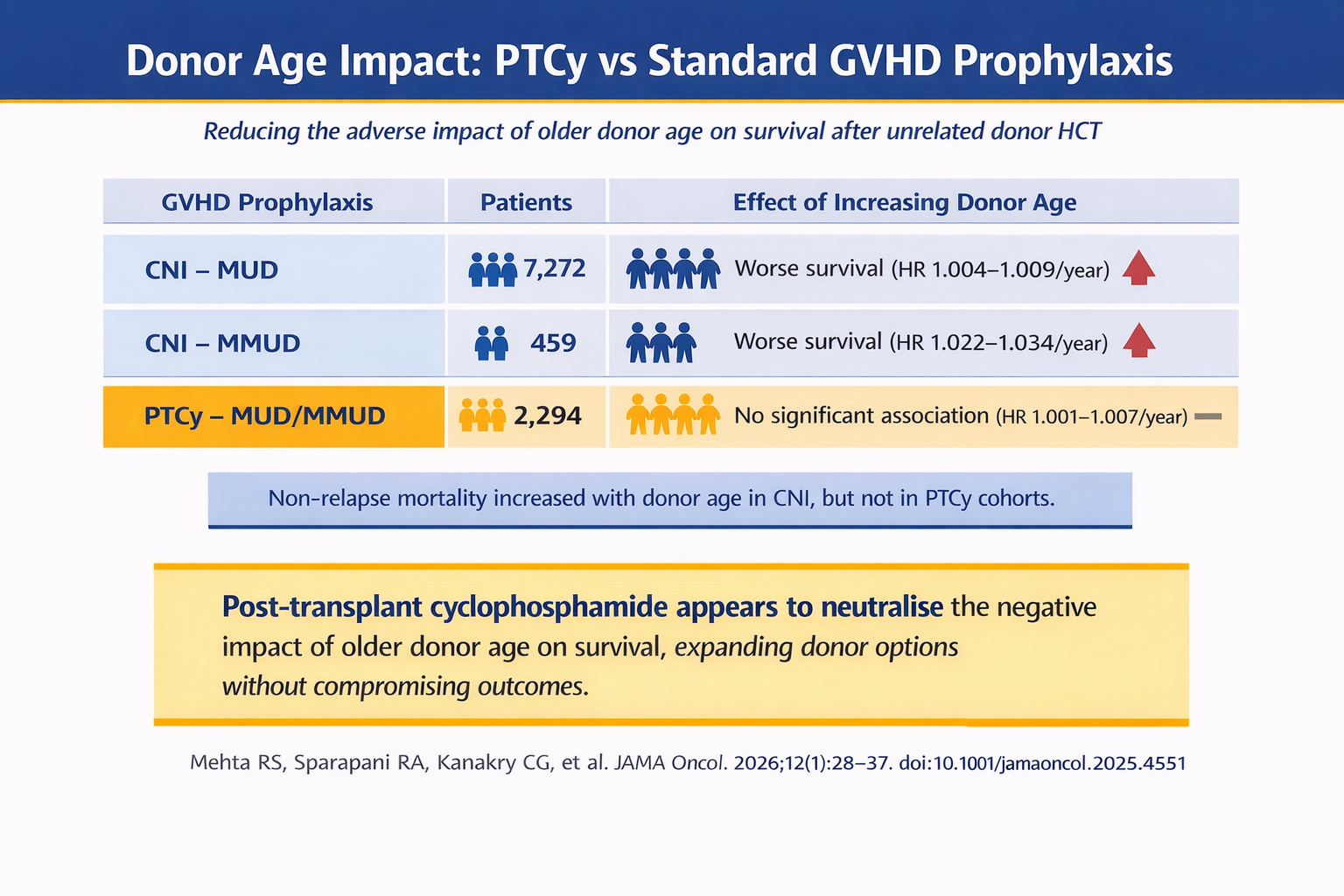
PTCy appears to mitigate the adverse impact of increasing unrelated donor age on post-transplant survival. In contrast to conventional CNI prophylaxis, older donor age did not significantly worsen outcomes when PTCy was used. This suggests that the longstanding emphasis on younger, unrelated donors may be less critical in the era of PTCy-based GVHD prophylaxis.
Why is this Relevant for South African Practitioners
In South Africa, where donor availability can be limited and transplant resources are constrained, understanding whether older unrelated donors remain a significant risk is crucial. This study suggests that using posttransplant cyclophosphamide may allow clinicians to safely expand the donor pool without compromising patient survival, informing donor selection strategies and optimising outcomes in local transplant practice.
Original Study
The content in this summary is intended as an overview only and does not replace the original research. Members should review the original study before forming clinical opinions. The Medical Education Network cannot be held liable for inaccuracies or omissions.
Fact-checking Policy:
The Medical Education Network makes every effort to review and fact-check source material. Please use the contact us form to report issues.


